Since the advent of genetic engineering, medicinal and biological chemistry have developed greatly, allowing for the development of drugs on the molecular level. One of the most beneficial development was the ability to create antibiotics. The ability of mankind to create antibiotics have cured many life-threatening illnesses caused by bacteria.
However, the misuse of antibiotics over the years have caused a significant problem to arise, which is the development of antibiotic resistance in bacteria. This has rendered many cures less effective, which means that previous illnesses that are though to be curable might not be useful as time goes on.
To understand the dangers of antibiotics misuse, we should first understand the underlying principles behind how bacteria and antibiotics interact with one another.
a
What are bacteria?

Fig 1: Bacteria of different shapes in microscopic level
Bacteria are prokaryotic organisms that are only a few micrometers in size and are small compared to eukaryotic cells.They generally appear in 3 different shapes- Spherical, Rod and Spiral. These organisms can be found almost everywhere except for places that have been sterilized thoroughly.
Bacteria that can survive in extreme conditions are known as extremophile. These bacteria are able to survive in places where humans cannot. For example, some bacteria can be found in lava, freezing polar regions and also deep underneath the ocean where pressure is high.
Bacteria can be categorized into heterotrophic and autotrophic. Herterotrophic bacteria consume other organism; either dead or alive while autotrophic bacteria uses photosynthesis or chemosynthesis to make food.
Bacteria can also be categorized into either Gram-positive or Gram-negative. Gram-positive bacteria have thicker peptidoglycan cell walls compared to gram-negative bacteria which have thinner peptidoglycan cell walls. This distinction is important to understand the pathogenic properties of bacteria. 90-95% of gram-negative bacteria are known to be pathogenic whereas most gram-positive bacteria tend to be non-pathogenic.
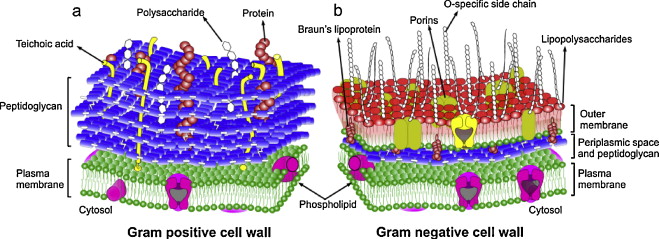
Fig. 1: General comparison of Gram-positive (a) and Gram-negative (b) bacterial cell wall structure
How exactly does bacteria infection cause illnesses?
Generally, when bacteria enters the body, they begin to multiply and damage the cells in the body. The body reacts to this change by showing signs and symptoms of illnesses.
Bacteria can attack the body in a number of ways. First, bacteria can multiply and crowd body tissues to disrupt normal functions. Second, bacteria can kill body cells and tissues by excreting chemicals that paralyzes the cell and third, they can react in the body to produce toxins.
What are antibiotics?
Antibiotics are medicines to treat infections/diseases caused by bacteria and parasites. Antibiotics can be taken orally, by injection or as creams, ointments or lotions to apply to skin. The discovery of antibiotics by Sir Alexander Fleming have saved many lives since it was first publicly used.
Antibiotics are categorized into either Narrow-spectrum or Broad spectrum. Broad spectrum antibiotics are effective against Gram-positive and Gram-negative while narrow-spectrum antibiotics are only effective against one category of the bacteria.
How do antibiotics work to cure illnesses?
Antibiotics essentially works in 3 ways:
- Disruption of peptidoglycan cell walls of bacteria causing cell burst
- Prevention of bacteria’s ability to grow
- Interruption of bacteria’s ability to repair DNA leading to eventual cell death
Below are some examples to demonstrate various antibiotic mechanisms:
- Beta-lactam antibiotics specifically target the cell wall of the bacteria by blocking the process by which bacteria combines molecules together. This causes the pressure in the cell to build up and eventually burst. Penicillin and cephalosporin are examples of beta-lactams.
- Macrolide antibiotics target the ribosomes in the cell of the bacteria. They prevent the ribosomes from producing proteins for the cell. Without proteins, the cell cannot to survive as proteins are the necessity to do work. Erythromycin is one of the example to treat skin infections.
- Quinolones antibiotics target the DNA replication mechanism of the bacteria. When the bacteria replicates DNA, quinolones breaks the DNA strands and stop the repairing mechanism. Bacteria cannot survive without a complete set of genome. Quinolones antibiotics are commonly used to treat pneumonia.
Is antibiotic treatment effective against all illnesses?
It is important to note that antibiotics do not work against all illnesses. Antibiotics are developed to work against the functions of pathogenic bacteria, as such, illnesses that are known to be caused by viruses are not curable by antibiotics. Some well-known illnesses caused by virus include cold, flu, HIV ,chickenpox and yellow fever.
Commonly, antibiotics are used to cure respiratory tract illnesses such as pneumonia and whooping cough, skin infections such as boils, styes and folliculitis and urinary tract infections such as yeast infection.
Also, antibiotics are designed specific to the species of bacteria being targeted. This means that there is no ‘one size fits all’ antibiotic. Depending on the type of bacteria being targeted, we would design specific antibiotic that can effectively target that bacteria.
What is antibiotic resistance?
Antibiotic resistance occurs when bacteria produces biological chemicals in response to the use of antibiotic medicines. These chemicals confers resistance against the specific antibiotic, allowing the bacteria to continue growing. This renders the antibiotic treatment ineffective as the ability of the antibiotic to control or stop bacterial growth is lost. These bacteria may then infect other humans and animals. The infections cause by these antibiotic resistance bacteria become harder to treat than those caused by non-resistant bacteria.
How does bacteria develop antibiotic resistance?
It is important to understand that bacteria do not suddenly develop resistance against antibiotics. The development of antibiotic resistance occurs due to the process of ‘natural selection’.
As a consequence of accumulated mutations in bacteria, some bacteria would already have antibiotic drug resistance. When bacteria is exposed to a antibiotic, those bacteria without resistance would be killed while those with resistance would continue to propagate. As such, it is expected that the new colonies of bacteria produced would all have antibiotic resistance. These new colonies of bacteria are then able to pass on their genes either through lateral transfer to other bacteria or vertical transfer to their offspring. This process repeats, allowing the antibiotic resistance gene to spread, even to other bacteria species.
The continued overuse of antibiotics thus speeds up the rate at which antibiotic resistance is set permanently into the genome of bacteria.
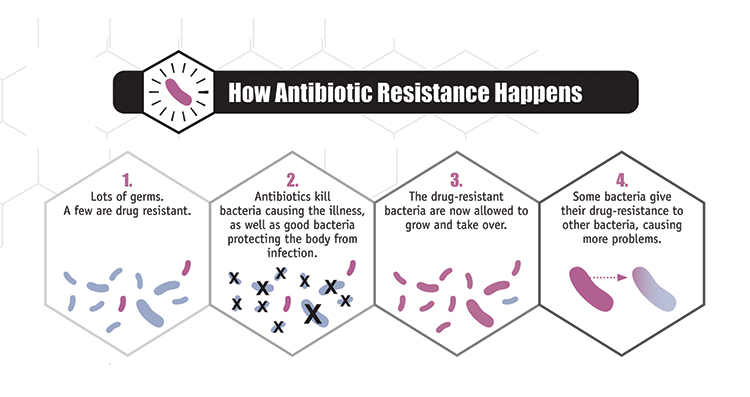
Fig. 2: Development of antibiotic resistance.
Some examples of antibiotic resistance development in bacteria
A growing list of infections that are becoming harder, and sometimes impossible, to treat as antibiotics become less effective.
- Resistance development in Salmonella and Campylobacter becoming more widespread primarily due to the use of antibiotics in food animals.
- Resistance development in E. coli against one of the most widely used medicines for the treatment of urinary tract infections (fluoroquinolone antibiotics) is becoming more widespread.
- Resistance development in Staphlylococcus aureus (a common cause of severe infections) against first-line drugs used to treat infections in health facilities is becoming more widespread.
- Resistance development in Klebsiella pneumoniae (common intestinal bacteria that can cause life-threatening infections ) against a last resort treatment (carbapenem antibiotics) has spread to all regions of the world. K. pneumoniae is a major cause of hospital-acquired infections such as pneumonia, bloodstream infections, and infections in newborns and intensive-care unit patients. In some countries, because of the resistance, carbapenem antibiotics do not work in more than half of the patients treated for K. pneumoniae infections.
- Resistance development in Neisseria gonorrhoeae has led to the failure of treatments using a last resort of medicine for gonorrhoea (third generation cephalosporin antibiotics). This has been confirmed in at least 10 countries (Australia, Austria, Canada, France, Japan, Norway, Slovenia, South Africa, Sweden and the United Kingdom of Great Britain and Northern Ireland). The new WHO guidelines do not recommend quinolones (a class of antibiotic) for the treatment of gonorrhoea due to widespread high levels of resistance.
- Resistance development in Enterobacteriacese against colistin has recently been detected in several countries and regions. Colistin is the last resort treatment for life-threatening infections caused by Enterobacteriaceae which are resistant to carbapenems. The development of antibiotic resistance has made infections caused by such bacteria untreatable.
- Resistance in Tuberculosis (TB): In 2014, there were about 480 000 new cases of multidrug-resistant tuberculosis (MDR-TB), a form of tuberculosis that is resistant to the 2 most powerful anti-TB drugs. Among new TB cases in 2014, an estimated 3.3% were multidrug-resistant. The proportion is higher among people previously treated for TB, at 20%. Extensively drug-resistant tuberculosis (XDR-TB), a form of tuberculosis that is resistant to at least 4 of the core anti-TB drugs, has been identified in 105 countries. An estimated 9.7% of people with MDR-TB have XDR-TB.
These cases are the proofs that antibiotic resistance development in bacteria have dire consequences.
In the next portion of this blog, we shall look into the ways in which society is affected and what should be done to resolve the issue of antibiotic misuse.
